Serial measurements of pro-BNP after acute coronary syndrome: risk marker?
Keywords:
NT-proBNP, Acute coronary syndrome, PrognosticAbstract
Increases in NT-ProBNP are markers of parietal stress and are caused by different mechanisms. Objective: To evaluate serial measurements of NT-proBNP in ACS and its relation to prognosis. Methods: Observational, prospective study that included 205 consecutive patients with acute coronary syndrome, hospitalized at the Institute of Cardiology of Corrientes from 01-JAN-2010 to 15-JAN-2011. The clinical, electrocardiographic, echocardiographic variables were assessed at baseline and one year. Blood samples were taken at baseline, 1 month, 6 months and 1 year, measuring NT-proBNP. Multivariate analysis was performed. Results: 25 pts (12.2%) unstable angina, 85 pts non-STEMI (41.4%) and 95 pts STEMI (46.4%). The mean age was 62.4±18 years, 78% male. The NT-proBNP values are shown in the attached Table.
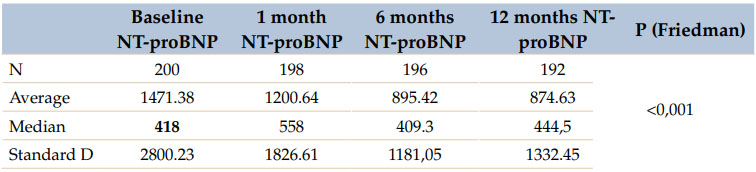
There was a significant diference between NT-proBNP at the baseline and at 1 month (p<0.001), 1 month to 6 months (p<0.001) and 6 months to 1 year (p<0.001). A multivariate model was constructed to see predictors in follow-up: troponin T persisted as an independent variable in the analysis, HR 3.5 (95%, CI 2.5-4.3), together with HF HR 3.2 (CI 95% 2.1-4.5), age HR 1.15 (CI 95%, 1.05-1.19) and NT-proBNP: HR 2.9 (IC 95%, 2.3-4.15). When ventricular remodeling was analyzed, a drop in ejection fraction (55.72 to 53.50%) was observed in patients in whom NT-proBNP levels remained high, p=0.01; and the diameter of the end of diastole increased (48.08 to 49.61 mm) p=0.03. The 2-year survival in patients who had 2 or more elevated NT-proBNP monitoring was 84% vs 92% for those with <2 determinations of elevated NT-proBNP (p=0.01). Conclusions: Patients with ACS who had 2 or more elevated NT-proBNP measurements had poor prognosis, related with ventricular remodeling manifested by lower ejection fraction and greater diameter of the left ventricle. Pro-BNP is an independent predictor of mortality during the follow-up.