Original Article
Correlation between the Killip-Kimball classification and the mortality of patients with ami, 55 years after its creation
Ferrero Lucas1, Di Cosco Oriana P1,
Grieve Santiago M1,
Bravo Lisandro D1, González Maria B1, Nebreda María C1, Milicich Gabriel A1,
Paolantonio Franco1,
Ovando Juan J1, Pompa Marina V1, Abraham Marcelo E1, Paolantonio Daniel L V2, Miraglia Edgardo D3.
1 Cardiology Service, Hospital Español de Rosario. 2 Coronary Care Unit Coordinator, Chief of Hemodynamic Service. 3 Chief of Coronary Care Unit, Chief of the Cardiovascular Ultrasound Department.
Corresponding author’s address
Dr. Ferrero Lucas
Postal address: Montevideo 927 1º B, 2000 Rosario, Santa Fe, Argentina
E-mail
INFORMATION
Received on March 16, 2022
Accepted after review
on August 10, 2022 www.revistafac.org.ar
There are no conflicts of interest to
disclose.
Keywords:
Acute myocardial infarction .
Heart failure .
Killip and Kimball - prognosis
ABSTRACT
Introduction: The Killip and Kimball (KK) classification was introduced in 1967 and clinically divides patients with acute myocardial infarction (AMI) according to the degree of heart failure on hospital admission. The objective of this study is to determine if there are differences between the subgroups and compare it with that presented in the original trial.
Material and methods: An analytical, retrospective, longitudinal and observational study of patients admitted for AMI to the coronary unit of the Hospital Español de Rosario over a period of 2 years was carried out. Subsequently, a comparative statistical analysis was performed between the subgroups according to the KK classification and of these results with those of the original Killip and Kimball clinical trial.
Results: There were 152 patients with AMI admitted, who presented an in-hospital and 30-day mortality since admission of 7.2%. In the comparative statistical analysis with that presented in the original work of KK (27.6%) a significant reduction is evident (P < 0.001). When evaluating mortality according to the KK classification, an increase was observed with a higher degree of heart failure presented on admission (Logrank test: P < 0.0001).
Conclusions: This survey shows that the classification of these patients according to the degree of heart failure presented on admission continues to be a prognostic marker of in-hospital mortality, retaining its clinical importance.
INTRODUCTION
The Killip-Kimball (KK) classification was introduced in 1967; it clinically divides patients with acute myocardial infarction (AMI) into four groups according to the degree of heart failure on hospital admission and it is described as an independent prognostic marker for mortality[1,2].
- Precordial pain suggesting cardiac ischemia, determined by the cardiologist responsible of the CCU.
- Alterations in electrocardiograms (ECG) made on admission and serially during the hospital stay, suggesting acute myocardial ischemia[3].
- New ST-segment elevation in J point in 2 contiguous leads of at least 1 mm in all leads, except for the V2-V3 leads, where the following cutoff points were applied: 2 mm in men ≥40 years; 2.5 mm in men <40 years or 1.5 mm in women regardless of age.
- New depression in horizontal or downsloping ST segment of at least 0.5 mm in 2 contiguous leads and/or T-wave inversion in 2 contiguous leads with prominent R wave or R/S ratio >1.
- Left bundle branch block. .
- Detection of a value of high-sensitivity troponin I above the 99th percentile of the upper limit of normality, and with a difference of at least 20% between measurement on admission and a second measurement 3 hours later[3]. .
On admission, they were classified into four groups, defined by Killip and Kimball according to the following characteristics:.
- KK A: Patient with no clinical signs of heart failure.
- KK D: Patient who is admitted due to cardiogenic shock (SBP <90 mmHg and signs of peripheral hypoperfusion)[1].
All patients coursed at least 48 hours of admission into the Coronary Care Unit of a tertiary medical center.
By a survey on digital clinical histories, the following data were recorded: history, type of coronary syndrome on admission: non-ST-segment elevation (NSTEACS), with ST-segment elevation (STEACS), location of AMI, ejection fraction measured by ultrasound during hospitalization, medical treatment established and revascularization method if performed: primary transluminal angioplasty (TCA) (performed on admission of patients with STEACS), urgent (performed during the procedure of urgent coronary angiography) or delayed (scheduled, whether during the procedure of diagnostic coronary angiography or at a second time) or coronary artery bypass grafting (CABG)[4,5]. Moreover, from the digital clinical history and the phone calls to relatives of patients, information was gathered on in-hospital mortality and 30 days after admission, on the total of the population studied.
Subsequently, a comparative analysis was made between mortality in the different KK subgroups, and with these results and those from the original clinical trial by Killip and Kimball[1]. For the statistical study, the IBM SPSS Statistics 2 software was used, with a 95% confidence interval (significant P of 0.05).
RESULTS
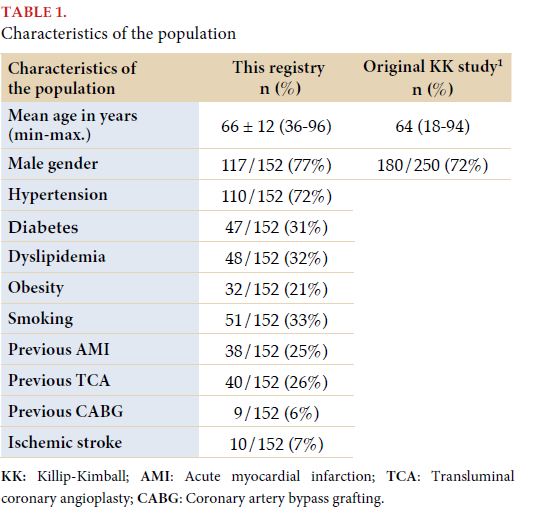
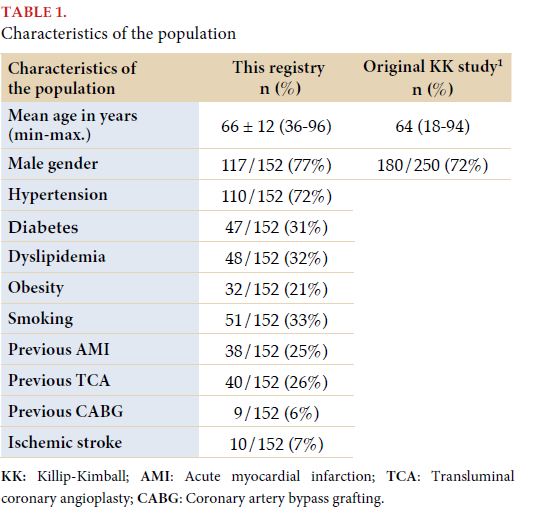
Data belonging to 152 patients were analyzed. The population characteristics are presented in Table 1.
When evaluating the usual medication, the following was observed: 33% received aspirin at the time of admission, 11% had a second antiplatelet drug (mainly clopidogrel), 58% was taking ACEI/ARBs, 30% beta blockers and 32% a statin.
NSTEACS is the most frequent diagnosis on admission, representing 57% of patients (n=87), with anterior/anterolateral compromise being predominant (37%). Ninety-two percent of patients admitted with NSTEACS underwent coronary angiography, of whom 31% presented significant lesions of 2 or more main coronary arteries, with the anterior descending artery as the one most frequently involved (43%). The rate of revascularization previous to discharge in patients with NSTEACS reached 78%, with predominance of delayed TCA (78%) in comparison to urgent TCA (16%) and CABG (6%) as revascularization method. In all cases, TCA coronary drug-eluting stent was implanted.
STEACS represents 43% (n=65), with anterior-anterolateral compromise being predominant, and the anterior descending artery being the most frequent culprit, reaching 43% of cases. Ninety-seven percent (63/65) was revascularized by primary TCA with coronary stent implant in the culprit artery during initial catheterization, not presenting complications that would force reintervention during the hospital stay. Within the KK D group, full revascularization was achieved in 6 out of 7 patients, with 1 case of death previous to admission to the hemodynamic laboratory. No patient underwent thrombolytic treatment for revascularization.
The medical treatment established during the stay in the CCU was made up by aspirin in 100% of patients, and a P2Y12 inhibitor in 99%, with clopidogrel being the most frequent (92%), followed by prasugrel (5%) and ticagrelor (3%). The rest of the indicated treatment during hospitalization and that was maintained until the discharge of the patient was: statins (100%), ACEI/ARBs (59%), beta blockers (90%), antimineralocorticoids (18%) and diuretics (12%), following the recommendations from STEACS and NSTEACS guidelines[4,5].
From all the patients admitted, ejection fraction (EF) measurements were made by Doppler echocardiogram within the hospital stay term in 97% (148/152). This measurement shows a mean EF of the total population of 51±14%. Between the patients who died during the hospital stay, the mean EF was 34%, while in survivors it was 52%.
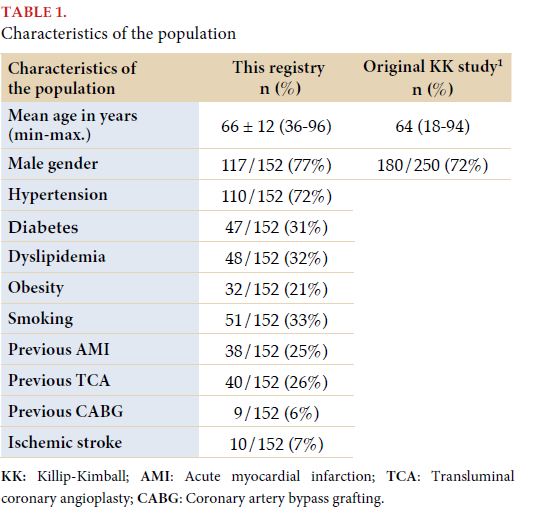
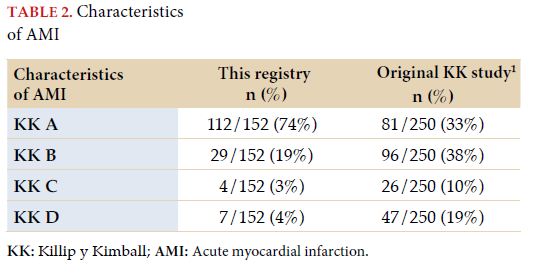
In Table 2, the distribution of patients admitted is shown, according to the degree of heart failure on admission as proposed by Killip and Kimball.
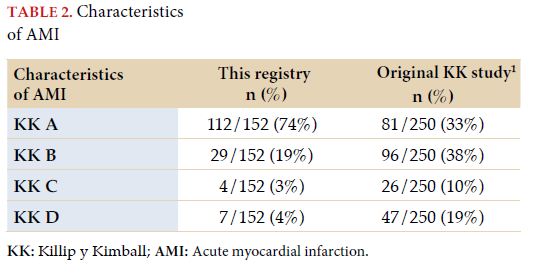
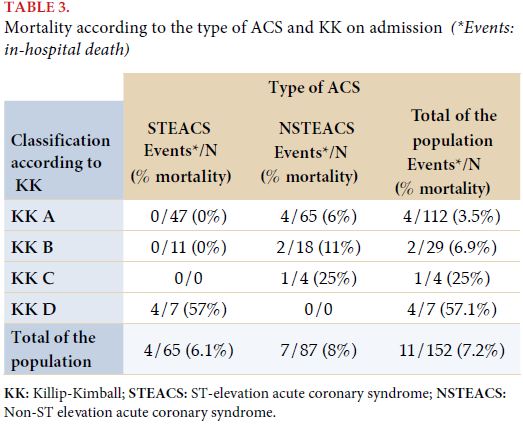
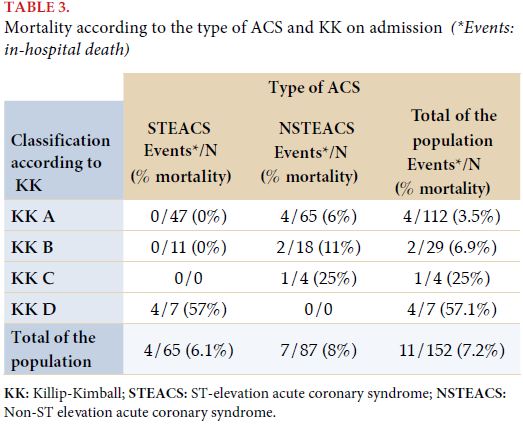
On the population analyzed, a total in-hospital mortality of 7.2% was recorded, with no differences with mortality in 30 days after admission. In Table 3, mortality is presented according to the type of acute coronary syndrome diagnosed on admission (STEACS or NSTEACS). When making the subanalysis according to type of ACS and KK classification, cardiogenic shock (KK D) was the only subgroup within patients with ST-segment elevation, who presented death during the hospital stay; while in patients with no ST-segment elevation on admission, there were no patients with cardiogenic shock and deaths occurred both in patients with and without signs of heart failure (the more incidence, the higher the degree of heart failure on admission).
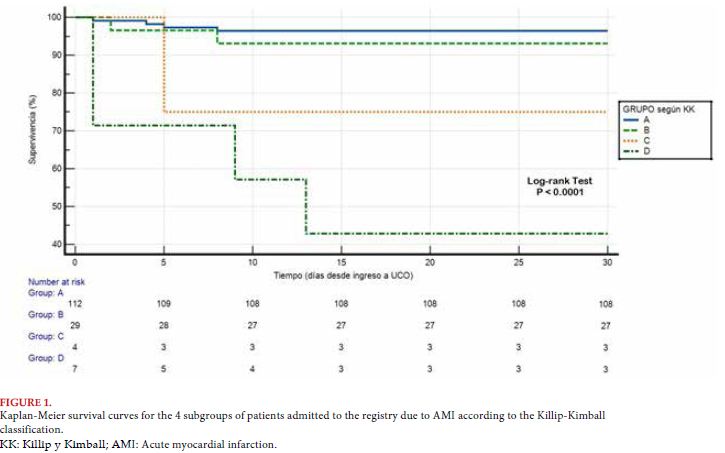
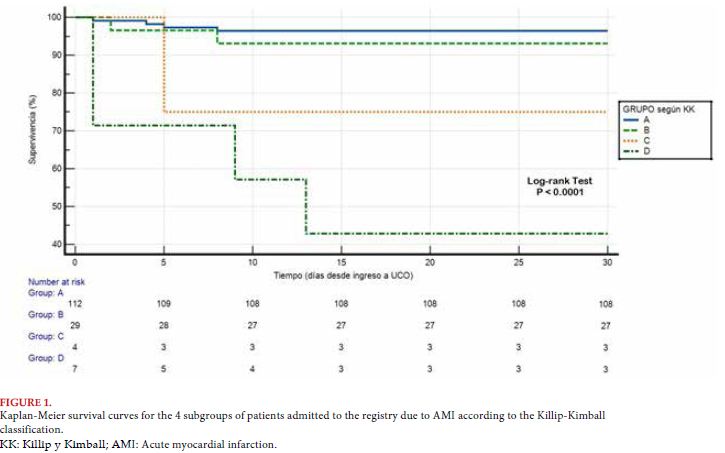
Analysis on survival within 30 days was made in the Killip and Kimball groups, which is observed in the Kaplan-Meier curves (Figure 1). This analysis showed a statistically significant difference in survival between the different KK groups (logrank test: P <0.0001), with more mortality, the higher the degree of heart failure presented on admission.
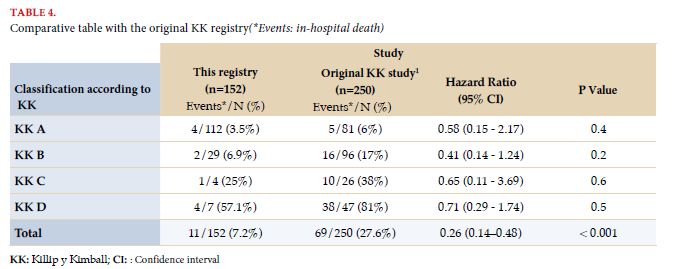
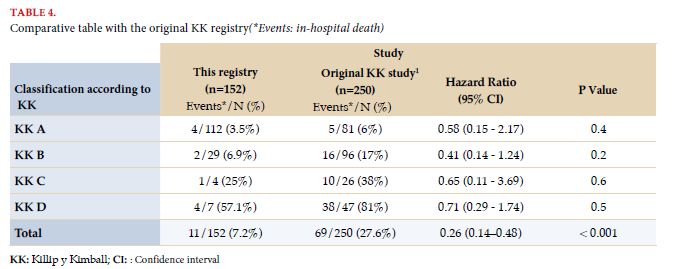
In Table 4, mortality is presented according to the KK classification and its comparison between this registry and the original KK trial[1]. In it, a relative 74% reduction is observed in overall in-hospital mortality in this registry (7.2%), in comparison with that presented in the original KK study (27.6%), which displays a high statistical significance (HR: 0.26; CI: 95%; 0.14 to 0.48; P <0.001)[1].
DISCUSSION
The 152 patients admitted represent 60.8% of the number of patients from the Killip and Kimball study from 1967 (250)[1]. It is important to highlight that half of the period analyzed corresponds to the 12 initial months of the Social and Compulsory Preventive Isolation decreed by the Ministry of Health due to the COVID-19 pandemic, where the number of admitted patients decreased..
The selection criteria used are due to the intent to resemble the population of the original study, which included patients with: clinical history compatible with AMI, changes in ST-T suggesting ischemia or appearance of diagnostic Q wave and increase in cardiac enzymes in serial measurements (GOT, GPT and LDH). Faced with the impossibility of using the same biochemical criteria (due to the lack of measurement curves for these enzymes), it was decided to replace them by troponin I measurement, current recommendation in the most recent international guidelines presented on the treatment for ST-elevation and non-ST elevation acute coronary syndrome[4,5]. Even so, no patients with cardiac enzyme alterations and with no alterations in ECG, or with alterations interpreted as of acute non-ischemic origin were included; nor patients who presented cardiorespiratory arrest before AMI diagnosis.
When comparing the population included in this Center with the one presented in 1967, it is possible to observe that mean age and male representation are similar. The information on previous medication is not available to make a comparison; but it is acknowledged we did not have most of the treatments used currently, which represents a significant difference between populations[6].
Another difference is evident in the hemodynamic characteristics of patients on admission: in this registry, 74% presented with KK A (n=114), 19% as KK B (n=29), 3% as KK C (n=4) and 4% with KK D (n=7); while in the original KK study there was a distribution of 33%, 38%, 10% and 19% respectively[1], which shows a decrease in the representation of groups C and D in this population, at the expense of an increase in the subgroup of patients with no heart failure on admission (group A). This decrease in the complication of AMI due to HF could be determined by multiple factors; between them, we could enumerate: early and timely care provided to patients with precordial pain (more awareness in society about the implications of chest pain) and increase in the diagnostic sensitivity of AMI with no heart failure (high-sensitivity troponin I measurement instead of GOT, GPT and LDH)[7].
The appearance of cardiogenic shock as a complication on admission was associated to patients with STEACS; while decompensated heart failure and acute pulmonary edema were more frequent in NSTEACS. Jointly, the proportion of patients with significant lesions of multiple vessels in coronary angiography was also more frequent between patients without ST elevation, which may account for the higher incidence of heart failure when faced with an acute coronary event and higher mortality associated[8].
Thanks to revascularization, dual antiplatelet therapy and the rest of the anti-ischemic treatment, the permeability of the culprit artery was reached in a high percentage of the sample, which reduces the possibility of presenting complications[9,10]. This may explain the statistically significant reduction of in-hospital mortality in this sample, in comparison to the original study, which is observed in all subgroups of the KK classification (with no significant individual differences, possibly by the small number of patients admitted in each subpopulation). In spite of all the changes introduced both in the diagnosis and the treatment of patients with AMI, a significant difference remains in mortality within 30 days between the patients in different KK groups on admission. Besides, the diagnosis of severe decrease in left ventricular ejection fraction during the hospital stay was associated to a higher risk of mortality. This correlates with what has been presented in different clinical trials, such as the one by Parakh et al. in 2008, showing the usefulness of left ventricular systolic function measurement as an independent predictor of mortality in patients with AMI[2].
The set of data analyzed and presented in this registry show that the usefulness of this classification presented by doctors Killip and Kimball in year 1965 remains valid, and is still a prognostic marker of mortality in patients with acute myocardial infarction[7,11,12].
CONCLUSIONS
This research study revalidates the usefulness of the classification according to the degree of heart failure presented on admission (Killip-Kimball classification) as a prognostic marker of patients with AMI. This simple practice maintains its correlation with in-hospital mortality and at 30 days, preserving its clinical significance after a significant decrease in the mortality of these patients after 55 years of medical advancements.
Acknowledgements
We would like to thank Guillermo J Bembibre MD, Chief of the Cardiology Service of the Hospital Español de Rosario, because of his constant encouragement and support; and Ariel R Quiroga MD, member of the Cardiology Service of the Hospital Español de Rosario, because of his selfless and essential collaboration.
BIBLIOGRAPHY
- Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary
care unit. Am J Cardiol 1967; 20: 457 - 464.
- Parakh K, Thombs BD, Bhat U, et al. Long-term significance of Killip class
and left ventricular systolic dysfunction. Am J Med 2008; 121: 1015 - 1018.
- Thygesen K, Alpert JS, Jaffe AS et al. Executive Group on behalf of the
Joint European Society of Cardiology (ESC)/American College of Cardiology
(ACC)/American Heart Association (AHA)/World Heart Federation
(WHF) Task Force for the Universal Definition of Myocardial
Infarction. Fourth universal definition of myocardial infarction. J Am Coll
Cardiol 2018; 72: 2231 – 2264.
- Collet J, Thiele H, Barbato E, et al. Guía ESC 2020 sobre el diagnóstico y
tratamiento del síndrome coronario agudo sin elevación del segmento ST.
Rev Esp Cardiol 2021; 74: 544 -544.
- Ibáñez B, Stefan J, Agewall S, et al. Guía ESC 2017 sobre el tratamiento del
infarto agudo de miocardio en pacientes con elevación del segmento ST.
Rev Esp Cardiol 2017; 70: e1 -e61..
- González-Juanatey RJ, Bermejo AR, López-Sendón J. Una historia resumida.
Impacto de los avances en cardiopatía isquémica. Rev Esp Cardiol
2017; (Supl 17): 2 – 6.
- Khot UN, Jia G, Moliterno DJ, et al. Prognostic importance of physical examination for heart failure in non-ST-elevation acute coronary syndromes: the enduring value of Killip classification. JAMA 2003; 290: 2174 -2181.
- DeGeare VS, Boura JA, Grines LL, et al. Predictive value of the Killip
classification in patients undergoing primary percutaneous coronary intervention
for acute myocardial infarction. Am J Cardiol 2001; 87: 1035
- 1038.
- Madias JE. Killip and Forrester classifications: should they be abandoned,
kept, reevaluated, or modified? Chest 2000; 117: 1223 - 1226.
- Weir RA, McMurray JJ, Velazquez EJ. Epidemiology of heart failure and
left ventricular systolic dysfunction after acute myocardial infarction:
prevalence, clinical characteristics, and prognostic importance. Am J Cardiol
2006; 97: 13F - 25F.
- Rovelli F, De Vita C, Feruglio GA, et al. GISSI trial: early results and late
follow-up. J Am Coll Cardiol 1987; 10 (Suppl B): 33B - 39B.
- Fu R, Song C, Yang J, et al. CAMI-NSTEMI Score - China Acute Myocardial
Infarction Registry-Derived Novel Tool to Predict In-Hospital Death
in Non-ST Segment Elevation Myocardial Infarction Patients. Circ J 2018;
82: 1884 - 1891.