1 Cardiologist, Clínica del Valle. 2 Cardiologist, Instituto de Cardiología de Corrientes “Juana F. Cabral”. 3 Hemodynamics Fellow, Fundación Favaloro. 4 Chief of Residents, Instituto de Cardiología de Corrientes “Juana F. Cabral”. 5 Clinical Cardiology Resident, Instituto de Cardiología de Corrientes “Juana F. Cabral”.6 Medical Staff, Service of Cardiovascular Recovery, Instituto de Cardiología de Corrientes “Juana F. Cabral”.7 Chief of Ultrasound Service, Instituto de Cardiología de Corrientes “Juana F. Cabral”.
Corresponding author’s address
Dr. Matías Gay Papp
Postal address: Bolívar 1334, 3400 Corrientes, Argentina
E-mail
Received on January 19, 2022 Accepted after review on June 13, 2022 www.revistafac.org.ar
There are no conflicts of interest to disclose.
Keywords:
Carotid artery stenosis .
Coronary artery disease .
Cardiovascular risk.
ABSTRACT
Introduction: Current records about the association between peripheral and carotid vascular disease with respect to coronary heart disease are at least 20 years old. For a decade there had been awareness that these records were old but were never updated at national level.
Material and methods:single-center, descriptive and observational registry. Primary endpoint: in-hospital and 30-day mortality; secondary endpoints: rate of peripheral and carotid artery disease in pre-coronary artery surgery patients; postoperative atrial fibrillation rate; readmission rate and mean number of days of hospitalization.
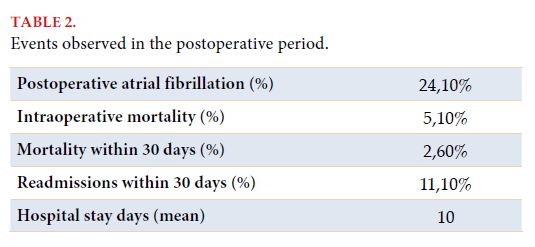
Results: Total of 239 pre-surgical coronary patients. Carotid artery disease in any of its severities occurred in 82%. The in-hospital mortality rate was 5.1%, and 2.6% at 30 days. A statistically significant relationship was demonstrated with mortality in terms of having any degree of injury in the external carotid (P: 0.01) and internal carotid (P: 0.045) arteries; except in the bulb (P: 0.1) and common carotid artery (P: 0.27).
Conclusions: Carotid artery disease in pre-surgical myocardial revascularization patients increases in-hospital mortality. No associations were found between mortality and readmissions with peripheral arterial disease.
INTRODUCTION
The patients with indication of myocardial revascularization surgery present association with coronary artery disease in other territories such as carotid arteries and lower limbs[1]. In fact, the Sociedad Argentina de Cardiología already recommends the screening and management of vascular diseases in multiple territories since the consensus on peripheral artery disease from year 2015[2]. In Argentina, two large multicenter registries on heart surgery were conducted: CONAREC III with 1,293 patients in year 1993; and the Estudio Multicéntrico de Cirugía Cardíaca (Multicenter Study on Heart Surgery - ESMUCICA) with 2,125 patients (which included patients with valve diseases) in year 1997. Both studies were made more than twenty years ago and present substantial differences to each other in the published results[3,4]. Considering medical and surgical advancements over recent decades, the need arose to make a new national, prospective and multicenter study to learn the characteristics, evolution, complications and mortality predictors of these patients. As there are few data currently, it was decided to make a single-center study. It is known that the association of comorbidities increases intraoperative morbimortality in operated coronary patients. In this study, not only the coexistence and significance of these comorbidities is highlighted, but also the implications in the perioperative periods, as well as immediate and 30-day mortality. .
Hypothesis: Panvascular disease adds morbimortality in coronary surgical patients.
Aims: To evaluate the implications on morbimortality of panvascular disease in coronary surgery patients.
MATERIALS AND METHODS
Single-center, descriptive and observational study. Patients were included with inclusion criteria from July 2017 to July 2020 at the Instituto de Cardiología de Corrientes “Juana F. Cabral”.
Inclusion criteria: patients older than 18 years, pre-surgical for myocardial revascularization surgery, who signed their informed consent.
Exclusion criteria: patients who did not present studies evaluating carotid artery disease.
Carotid artery disease was defined as the presence of any carotid artery lesion from mild atheromatosis to occlusion, in any territory of the carotid arteries and its branches, whose diagnosis could be made both by arterial Doppler ultrasound or neck angiography. Literature divides them into mild, moderate and severe.
Peripheral disease of lower limbs was defined as the presence of mild or major plaque in any arterial vascular territory of lower limbs measured by angiography. The amputation of lower limbs was defined as any amputation of lower limbs.
Endpoints:
Primary:
1. In-hospital and 30-day mortality.
Secondary:
1. Peripheral artery and carotid artery disease rate in patients pre-coronary surgery;
2. Postoperative atrial fibrillation rate;
3. Readmission rate;
4. Mean of hospital stay days.
Statistical analysis:
Continuous variables were compared by student’s t-test (or Mann-Whitney U test); categorical variables by chi-squared test. A p value <0.05 was considered statistically significant. All statistical analyses were made with the SPSS 21.0 software (SPSS Inc, Chicago, Il). Variants were compared in each of the vascular diseases.
RESULTS
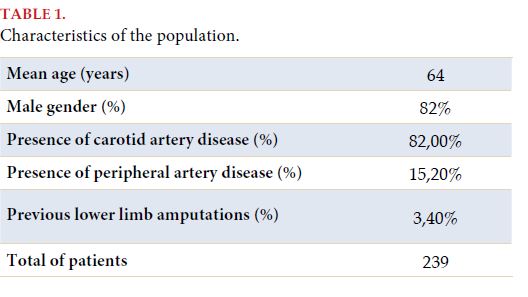
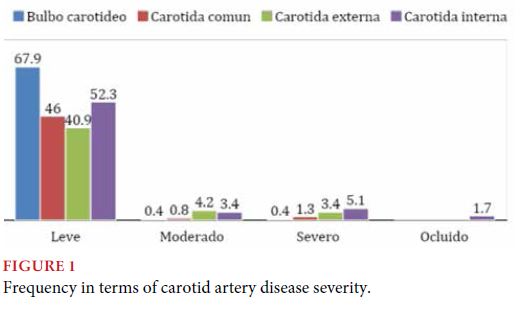
In this registry, 239 pre-coronary surgery patients were included, whose characteristics are detailed in Table 1.
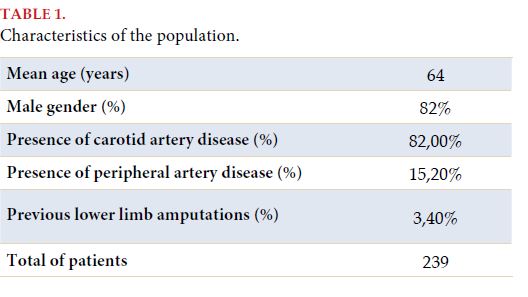
Carotid artery disease in any degree of severity presented in 82% of the population studied, although in most cases, it was a mild disease and located on the carotid bulb (Figure 1).
DISCUSSION
The association between CAD and vascular disease in other territories was clearly shown in this study. The presence of carotid artery and peripheral artery disease was observed in 82% and 15.2% respectively in the population studied. This is not new, as in the CONAREC XVI registry, the most recent registry on this topic, 9.56% of peripheral vascular disease was verified in patients who underwent coronary surgeries. Also, 4.93% of mortality was also observed, in comparison to this study, where in-hospital mortality was 5.1%[1].
Although the association with carotid artery disease was relevant, more specifically in territories in the external and internal carotid arteries, in at least a mild degree, it is possible to state that this study will be limited in terms of the number of the population in comparison to other registries at national level. It is possible to infer that the result may have been higher, if the population had been more extensive. It is true that the significance of carotid artery disease was verified, in any degree of severity, in relation to the outcome for patients who undergo coronary surgery.
LIMITATIONS OF THE STUDY
No routine tests were made to detect peripheral artery disease; the patients that had tests made were due to the presence of symptoms, or previous lower limb amputations. This is due to the detection of lower limbs peripheral artery disease not being part of institutional preoperative screening.
Cardiovascular risk factors were not taken into account for the association of mortality and peripheral artery disease, which raises the question of possible subsequent studies or registries, associating the disease with risk factors.
CONCLUSIONS
The presence of carotid artery disease in preoperative patients for myocardial revascularization surgery increases in-hospital mortality. No associations between mortality and readmissions were found in regard to peripheral artery disease with previous lower limb amputations.
BIBLIOGRAPHY